Allergy Blood Test Could Identify Risk of Rare COVID-19 Vaccine Reaction
A study shows a popular allergen test may help identify patients at risk of allergic reaction to a compound found in COVID-19 mRNA vaccines.
By
Kevin Kunzmann
| Published on September 24, 2024
4 min read
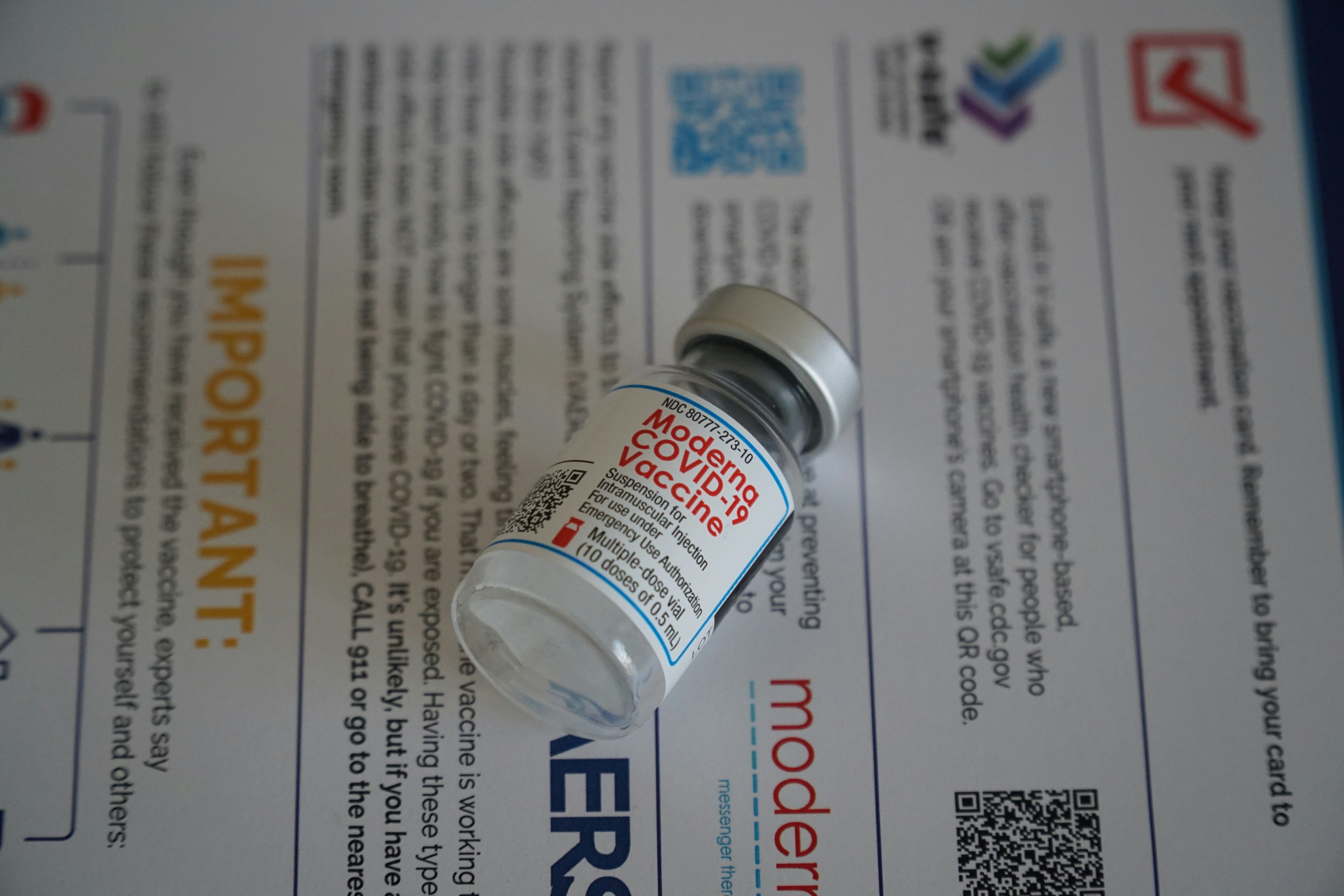
Credit: Unsplash / Ian Hutchinson
The basophil activation test (BAT), a diagnostic strategy that assesses white blood cells involved in allergic reactions, conducted with a popular formula of the COVID-19 vaccine could help identify sensitization to polyethylene glycol (PEG) in patients with PEG allergy.
The findings from the new clinical trial suggest that allergy workups may consider including a BAT diagnostic to convey patients’ allergy to PEG, as the synthetic compound becomes increasingly present in lipid nanoparticulate formulas that make up advanced medical products such as the COVID-19 mRNA vaccines. Namely, if more vaccines and therapies are to include formulary PEG in the future, these data suggest it’d be ideal to test for any allergies or sensitizations to it through a BAT diagnostic.
Aside from mRNA vaccines, PEG is used in various ways for pharmaceutical and cosmetic products—including as a thickening agent for moisturizers, as well as a solvent or stabilizer in drugs and therapeutic proteins. In mRNA vaccines, the compound plays an incremental role in lipid nanoparticle encapsulation. However, concerns have been raised about the risk of allergic reactions to PEG. Research has shown a “small fraction” of people to receive the Pfizer-BioNTech or Moderna COVID-19 vaccines (Comirnaty and Spikevax, respectively) experience a hypersensitivity or anaphylactic reaction to the PEG compound.
BAT is often used to detect immunoglobulin E (IgE)-mediated allergies from high-risk foods and drugs through a blood sample that isolates basophils and exposes them to concentrations of the suspected allergen. The rate of increased activated basophils in response to an allergen versus a non-allergen (control) can help provide a clinical allergy diagnosis.
Investigators from Germany conducted a small-scale study of 20 patients to observe the sensitivity of BAT in detecting sensitization to PEG in patients previously diagnosed with a PEG allergy, using the Pfizer-BioNTech Comirnaty vaccine as reference. The participant pool included 10 patients with PEG allergy and 10 healthy controls; blood tests from the participants were used to assess four different concentrations of the COVID-19 vaccine.
Investigators found that basophil activation was significantly greater in the blood tests of patients with a PEG allergy versus that of the control participants, meaning the BAT may help indicate a high sensitization to PEG relevant to the COVID-19 mRNA vaccines. The data showed a 60 percent sensitivity and 100 percent specificity for PEG with the BAT diagnostics—meaning that 6 of the 10 patients were correctly identified as being allergic to PEG, and all 10 patients were correctly identified as not a false positive for the allergy.
As PEG becomes a more prominent feature of mRNA vaccines, cancer immunotherapies and other clinical innovations, more cases of PEG-allergic reactions to treatment may occur in patients. Folding BAT diagnostics into allergy workups may help reduce the risk of anaphylaxes or other allergic side effects in most individuals based on these findings.
“Although PEG allergy has a low prevalence, allergological work-up of PEG allergic patients including BAT with PEG lipid nanoparticles might play a role in the future when these substances will be used not only for vaccination, but also for cancer immunotherapies,” the investigators concluded.
References
- Eberlein, B., Mathes, S., Darsow, U., Biedermann, T., & Brockow, K. (2024). Allergy to PEG (polyethylene glycol) – sensitivity of basophil activation test with COVID-19 mRNA-vaccine BNT162B2. Human Vaccines & Immunotherapeutics, 20(1). https://doi.org/10.1080/21645515.2024.2312600
- Kozma GT, Mészáros T, Berényi P, et al. Role of anti-polyethylene glycol (PEG) antibodies in the allergic reactions to PEG-containing Covid-19 vaccines: Evidence for immunogenicity of PEG. Vaccine. 2023;41(31):4561-4570. doi:10.1016/j.vaccine.2023.06.009

